Every day, millions of people wake up with stiff joints, chronic fatigue, or mysterious aches that don’t seem to go away. For many, these symptoms signal more than aging, they may point to a rheumatic disease. As a specialty, rheumatology helps us understand, diagnose, and manage the more than 100 conditions that affect joints, muscles, bones, and connective tissues, many of which are autoimmune disorders.
Our goal in this article is to demystify rheumatology. By the end, you’ll have a comprehensive understanding of what these diseases involve, signs to look for, diagnostic steps, and the latest treatments available to help patients live better, more mobile lives. Whether you’re managing symptoms or assisting a loved one, you’re in the right place.
Rheumatic diseases are chronic, often progressive conditions that primarily affect the musculoskeletal system, but can also impact internal organs, skin, and the immune system. These diseases fall largely into two categories: inflammatory autoimmune diseases, like rheumatoid arthritis and lupus, and degenerative conditions like osteoarthritis.
What makes these conditions particularly complex is their systemic nature. Rheumatic diseases don’t just affect one body part. They may progress silently for years, sometimes confusing both patients and primary care providers with symptoms like fatigue, low-grade fevers, skin rashes, and alternating periods of flares and remission.
Chronic inflammation from these diseases can lead to joint damage, loss of mobility, reduced quality of life, and even life-threatening complications if untreated. This is why early diagnosis and intervention are crucial.
Let’s take a closer look at some of the most frequently diagnosed rheumatic diseases:
Affecting around 0.5% to 1% of the global population, RA is an autoimmune disorder where the immune system mistakenly attacks joint linings. Key symptoms include:
The most common form of arthritis, OA results from cartilage wear-and-tear. It’s non-inflammatory but can still impair movement:
This autoimmune condition affects joints, skin, kidneys, and more:
Found in people with psoriasis, this disease combines skin and joint symptoms:
Gout is often associated with uric acid buildup, producing sudden flare-ups in specific joints. AS primarily affects the spine and sacroiliac joints.
Our joints speak before our mouths do, recognizing these early signals can prompt timely consultation with a rheumatologist.
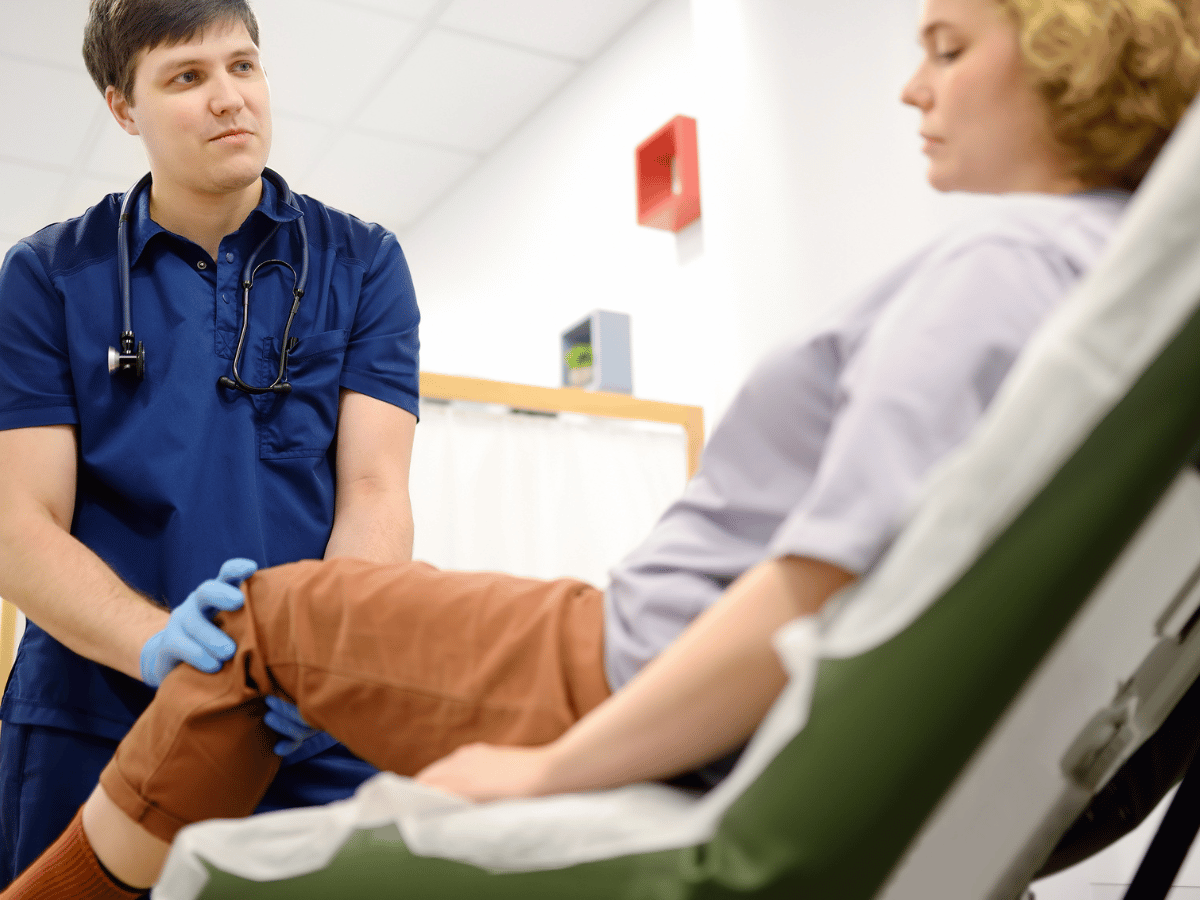
An accurate diagnosis requires a detailed history, physical exam, lab work, and sometimes imaging. Rheumatologists start by listening and asking about your symptoms, their onset, patterns, and family history. The next steps often include:
Starting treatment early, within 3-6 months of symptom onset, can prevent up to 50% of permanent joint damage in conditions like RA. That’s a life-changing statistic.
Treatment in rheumatology is increasingly personalized. Here’s how we categorize them:
These drugs slow disease progression and prevent joint damage. Methotrexate, widely used for RA, is often first-line.
More targeted than traditional DMARDs, biologics like TNF inhibitors and IL-6 blockers have revolutionized rheumatology. They’re especially helpful when conventional therapies fall short.
These newer drugs like Janus kinase (JAK) inhibitors block specific cellular pathways to calm immune overreaction.
NSAIDs and corticosteroids are still used to manage flares or serve as bridge therapies before DMARDs take effect.
Medications do the heavy lifting, but comprehensive care includes much more:
Custom movement plans improve mobility, protect joints, and reduce stiffness. Therapists often work alongside rheumatologists to tailor regimens safely.
An anti-inflammatory diet, rich in omega-3s, leafy greens, and whole grains, can mitigate flare-ups. Maintaining a healthy weight also reduces strain on joints.
Depression and fatigue are common in chronic illness. Support groups and behavioral therapies provide emotional resilience and coping strategies.
We’re in a transformative decade for rheumatology. Precision medicine, matching treatments to genetic or biomarker profiles, is moving from theory to practice. Research is also looking into:
Clinical trials are expanding access to experimental therapies for those with resistant disease patterns.
Don’t wait until symptoms intensify. Early signs that deserve rheumatologic attention include:
The future of rheumatology is patient-centered and tech-enabled. We’re heading toward a world where therapies are tailored to your immune system profile, wearable tech flags flares before they start, and AI helps predict disease progression.
But perhaps the most transformative change? Empowered patients. Education and public awareness allow people to advocate for diagnosis earlier and manage their symptoms with confidence.
If you or someone you care about experiences chronic joint pain, stiffness, or unexplained fatigue, don’t wait. These may be signs of an underlying rheumatic condition. At South Florida Multispecialty Medical Group, our rheumatology experts combine cutting-edge diagnostics with compassionate care. Schedule a consultation today, and take the first step toward relief and restored mobility.
Rheumatology is a medical specialty focused on diagnosing and managing diseases that impact the joints, muscles, bones, and immune system. It includes conditions like rheumatoid arthritis, lupus, osteoarthritis, gout, and psoriatic arthritis.
Rheumatic diseases are widespread. Rheumatoid arthritis affects about 0.5%–1% of the global population. Osteoarthritis is even more common, affecting millions worldwide, especially older adults.
Symptoms vary but often include joint pain, stiffness (especially in the morning), swelling, fatigue, redness, and restricted movement. Some autoimmune diseases may also cause skin rashes, ulcers, and fever.
Diagnosis typically involves blood tests (like rheumatoid factor, anti-CCP, ANA), imaging studies (X-rays, MRIs, ultrasound), and lifestyle evaluations. Rheumatologists combine several tools for accurate diagnosis.
Biologics and DMARDs slow down or stop disease progression. They control inflammation, reduce joint damage, and improve function. They're especially helpful in conditions like RA and lupus.
If joint pain, stiffness, or swelling persist for more than a few weeks—especially with fatigue, unexplained fevers, or skin changes—it’s time to see a rheumatologist.
Treatments include DMARDs, biologics, NSAIDs, corticosteroids, physical therapy, and lifestyle changes such as diet and exercise. Newer targeted drugs like JAK inhibitors are also effective.
Yes. Anti-inflammatory diets, regular low-impact exercise, smoking cessation, weight control, and stress management all play important roles in managing symptoms and improving quality of life.
Your well-being is our top priority. Reach out today to discover how our dedicated team can support your health journey.
Have questions or want to learn more? Use the form below to get started!
Connect with South Florida’s trusted multispecialty care team and take control of your health with compassion and convenience.
©2025 South Florida Multispecialty Medical Group. All Rights Reserved.