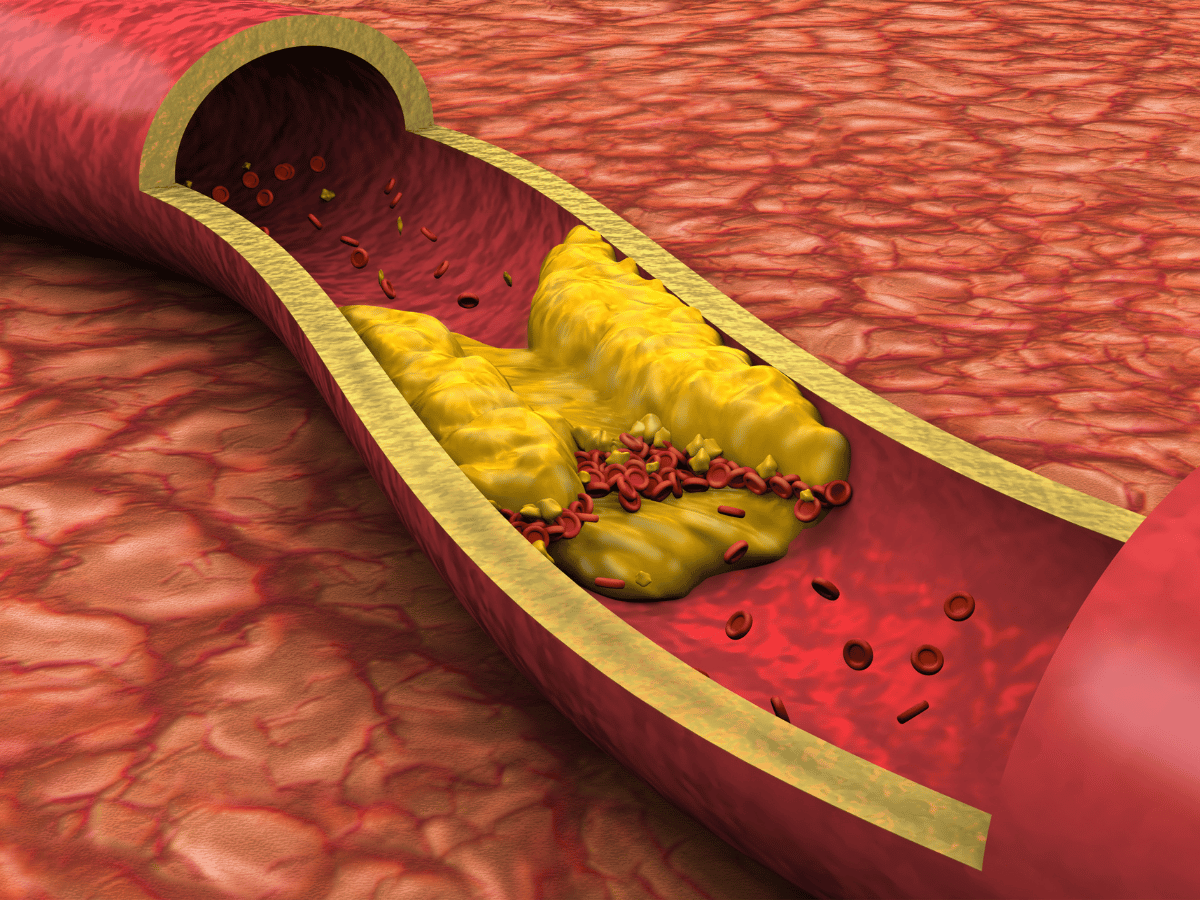
Peripheral Arterial Disease, or PAD, is a condition in which arteries, specifically those supplying the limbs, become narrowed due to plaque buildup (atherosclerosis). This process hinders proper blood flow, particularly to the legs. When tissues don’t get enough oxygen-rich blood, symptoms begin to emerge, the most telling of which is leg pain during walking, known as intermittent claudication.
PAD is not a vein disorder; it’s exclusively an arterial problem. Recognizing this distinction is important, especially since terms like PAD and PVD (Peripheral Vascular Disease) are sometimes used interchangeably. Let’s set the record straight below.
PAD refers specifically to arterial disease, meaning the problem lies in arteries that carry oxygen-rich blood away from the heart to the rest of the body, particularly the legs. On the other hand, PVD is a broader term that encompasses all diseases of blood vessels, including both arteries and veins. So, while all PAD is PVD, not all PVD is PAD.
This matters clinically because the treatment approach, potential risks, and long-term outcomes differ. Vein diseases are typically not caused by atherosclerosis and respond to different therapies compared to PAD. If we’re managing PAD, we’re tackling artery-related issues; it has nothing to do with varicose veins or venous insufficiency.
Atherosclerosis is the buildup of plaque inside arterial walls and it is by far the most common cause of PAD. These plaques are composed of cholesterol, fat, and other cellular debris that cause arteries to narrow and stiffen over time.
Risk factors include:
These risk factors damage the endothelium (arterial lining), paving the way for atherosclerosis to develop and advance silently until symptoms show up.
Intermittent claudication is one of the hallmark symptoms of PAD. It’s best described as cramping, aching, or fatigue in the legs triggered by walking or exertion and relieved by rest.
Imagine someone walking down the street and having to stop every block because their calves tighten painfully. That’s claudication. As PAD worsens, the symptoms can progress to pain at rest, non-healing sores, and even gangrene.
Additional symptoms may include:
These signs aren’t just discomforts, they’re red flags. Early intervention leads to significantly better outcomes and often avoids progression to severe, limb-threatening stages.
We use multiple noninvasive and minimally invasive tests to confirm PAD:
A good clinical exam remains foundational, especially pulse palpation in the feet and signs of trophic changes on the skin (e.g., hair loss, color changes).
The risks of ignoring PAD are steep. As the arteries narrow more seriously, patients may develop:
One of the biggest misconceptions is that PAD is purely a leg issue. In reality, it’s a tip of the iceberg problem that signals widespread vascular disease.
PAD treatment is multifactorial. Our approach focuses on four major pillars:
Some patients need more than lifestyle and meds. For advanced cases or when standard therapy isn’t enough, we turn to revascularization strategies:
Endovascular methods have evolved quickly, offering minimally invasive options with shorter recovery times compared to traditional vascular surgery.
Preventing PAD or preventing its return is all about controlling the controllables. We educate our patients to:
Even after successful treatment, PAD can recur. Long-term success depends on lifelong commitment, something we guide our patients through with continued support.
While PAD can feel limiting at first, many patients regain mobility and improve health with proper care. We’ve seen people go from barely making it down a driveway to hiking again after structured rehab and intervention.
The key lies in early diagnosis, personalized treatment plans, and routine follow-up. Combining risk control with medical or procedural management gives most people their life and their legs back.
If you’re experiencing leg pain while walking, numbness, foot discoloration, or wounds that won’t heal, it’s time to speak with a vascular specialist. Early detection means better outcomes and preventing the catastrophic complications of untreated disease.
Our team at South Florida Multispecialty Medical Group is equipped with the tools and experts needed to not just diagnose PAD, but to personalize your path to recovery.
If you’re experiencing leg pain while walking, wounds that won’t heal, or numbness in your lower limbs, don’t wait. Contact the vascular experts at South Florida Multispecialty Medical Group today. Early diagnosis and treatment can protect your mobility and your life.
PAD is a circulatory condition where arteries, particularly in the lower limbs, become narrowed due to plaque buildup, causing restricted blood flow.
Smoking, diabetes, high blood pressure, elevated cholesterol, obesity, and a sedentary lifestyle are leading risk factors.
Look for intermittent leg pain while walking (claudication), cold feet, wounds that don't heal, or noticeable limb weakness.
PAD is commonly diagnosed through physical exams, the ankle-brachial index (ABI), ultrasound studies, and sometimes CT or MR angiography.
Treatment spans lifestyle changes, medications like antiplatelets and statins, supervised exercise therapy, and in some cases, surgical or endovascular procedures.
Yes. PAD raises the risk of heart attacks, strokes, and severe limb complications including ulcers, infections, and amputation.
Quit smoking, exercise regularly, eat a healthy diet, and keep chronic conditions like hypertension and diabetes under tight control.
See a specialist if you experience leg cramps after walking or resting leg pain, as prompt treatment can prevent serious complications.
Your well-being is our top priority. Reach out today to discover how our dedicated team can support your health journey.
Have questions or want to learn more? Use the form below to get started!
Connect with South Florida’s trusted multispecialty care team and take control of your health with compassion and convenience.
©2025 South Florida Multispecialty Medical Group. All Rights Reserved.