Modern medicine has revolutionized the way we manage serious cardiovascular risks, particularly in patients where standard treatments like anticoagulants aren’t an option. An example of such innovation is the Inferior Vena Cava (IVC) filter. It’s a small device with a big impact: preventing deadly blood clots from traveling to the lungs.
South Florida, like many regions with a diverse and aging population, sees its fair share of deep vein thrombosis (DVT) and pulmonary embolism (PE) cases. Many lives have been saved thanks to timely filter placements. But as with all interventions, timing, technique, and thoughtful follow-up care make all the difference. So let’s walk through what every patient and provider should know about IVC filters.
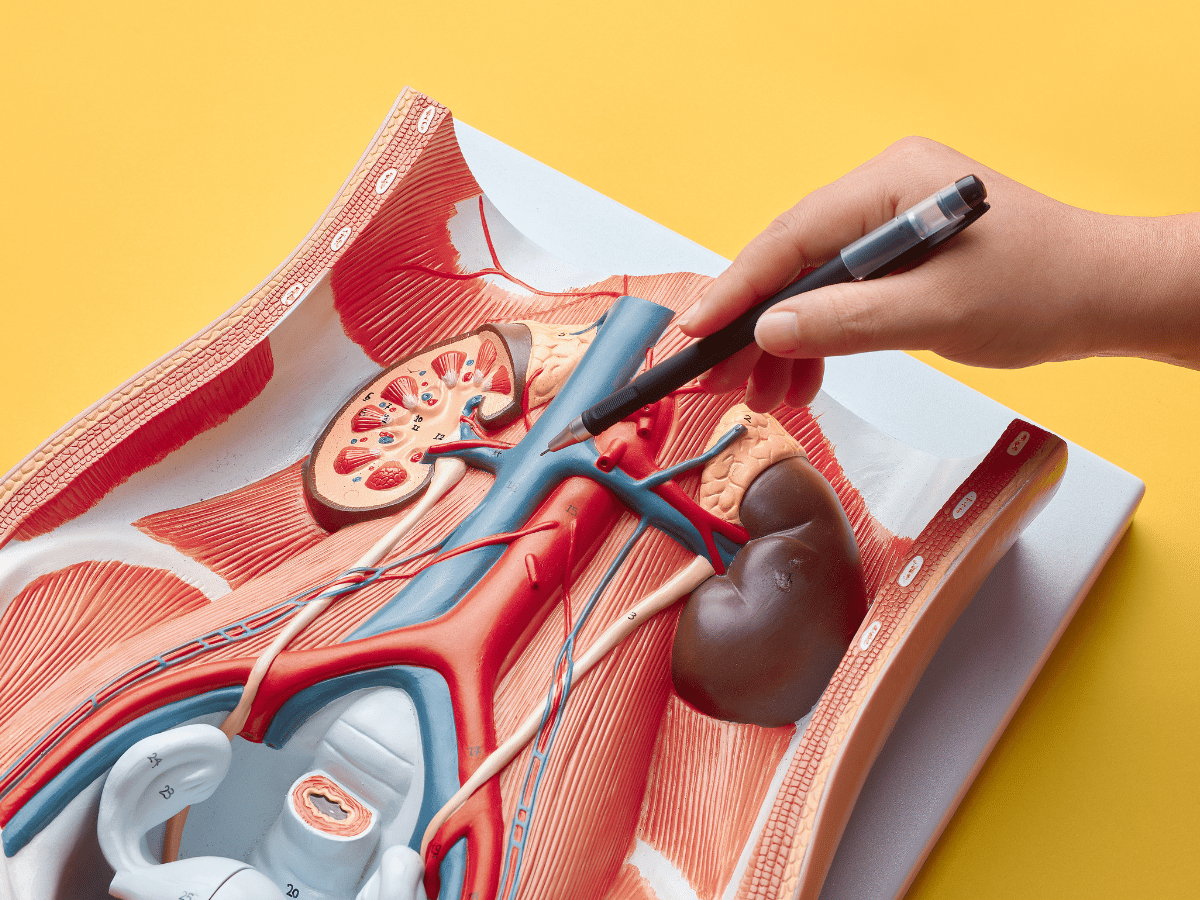
The inferior vena cava (IVC) is the largest vein in the body, carrying blood from the legs, pelvis, and abdomen back to the heart. An IVC filter is a small, cage-like device placed in this vein to catch blood clots, essentially acting as a barrier to prevent them from reaching the lungs, where they could cause a pulmonary embolism.
These filters don’t dissolve clots but trap them so the body’s natural system can break them down over time. They’re designed to help patients at high risk who either can’t use blood thinners or for whom these medications haven’t worked.
We typically recommend IVC filters in one of three cases:
The decision isn’t taken lightly. Specialists from hematology, interventional radiology, and vascular surgery typically collaborate to determine appropriateness.
Placement is a minimally invasive procedure. It usually takes less than an hour and is done under local anesthesia with mild sedation. Here’s how it goes:
Once secure, the filter begins working immediately to trap emboli moving toward the lungs, reducing the risk of a life-threatening PE.
While anticoagulants are typically the first line of defense, filters offer a critical safety net when medications are not an option.
Key benefits include:
One South Florida case involved a trauma patient who had suffered multiple fractures and internal bleeding. Anticoagulation was too risky. An IVC filter was placed, and clots were later detected in the filter, proof that it likely prevented a fatal PE.
As with any medical device, IVC filters are not without risks, especially when left in place indefinitely. That’s why proper follow-up is crucial.
These risks emphasize why retrievable filters should be removed once they’re no longer needed.
Historically, retrieval was considered easy only within the first few weeks after placement. Today, retrieval techniques have progressed, making it possible even after months or years.
Interventional radiologists now use advanced methods such as loop snare techniques, laser-assisted retrieval, or complex endobronchial forceps in tough cases.
According to the Journal of Vascular and Interventional Radiology, the retrieval success rate exceeds 95% when managed by experienced specialists, an encouraging statistic for practitioners and patients alike.
When the time is right, filter removal is just as crucial as placement. The retrieval is usually done under local anesthesia with light sedation.
Post-removal, we monitor patients for several hours, checking for signs of bleeding or complications. Most go home the same day.
Here’s something we can’t stress enough: Follow-ups save lives.
After placement, patients need regular check-ins to assess risk factors, evaluate the filter’s position, and determine the best window for retrieval. Unfortunately, data shows that many temporary filters stay in longer than necessary, an avoidable risk.
Hospitals like South Florida Multispecialty utilize dedicated filter tracking programs. These help ensure timely reminders for both patients and referring physicians, improving safe filter removal rates significantly.
Most modern filters are retrievable, but not all are removed. Some patients still need long-term protection.
Choosing between the two depends on a patient’s specific health profile and clotting risks.
IVC filters are a powerful tool in the fight against deadly pulmonary embolism, but only when used thoughtfully and removed at the appropriate time. Their value lies not just in placement, but in the entire continuum of care surrounding them.
At South Florida Multispecialty Hospital, we take pride in offering coordinated care that prioritizes accurate indications, skilled placement, diligent monitoring, and expert filter retrieval.
Ready for expert guidance? Connect with our vascular team to assess your risk profile and explore if an IVC filter might be the right step for you or whether it’s time to safely remove one.
If you or a loved one has been diagnosed with DVT or is living with an IVC filter, it’s time to consult with our experts at South Florida Multispecialty Hospital. Don’t wait, get the personalized care you need today.
An IVC filter is a device placed in the large vein that returns blood from the lower body to the heart. It prevents blood clots from traveling to the lungs, often used when blood thinners can’t be prescribed.
Patients with deep vein thrombosis or pulmonary embolism who can’t safely take anticoagulants or who have recurrent clots despite medication may need a filter.
The procedure involves inserting a catheter into a vein, typically in the groin or neck, and guiding the filter into the inferior vena cava using X-ray imaging. It’s minimally invasive and often completed in under an hour.
Removal involves snaring the filter via a catheter and gently retracting it through the vein. It’s typically done once the patient no longer needs clot protection, often within weeks to months after placement.
Risks include device migration, vein perforation, filter fracture, or clot formation around the filter itself. Long-term use without monitoring increases these risks.
Temporary filters are often intended to remain in place for a few weeks to a few months. Some are left in longer based on ongoing clot risk. Regular imaging helps determine timing.
Yes. Anticoagulation remains the first-line treatment. Compression stockings and early ambulation are also supportive measures for DVT prevention.
Follow-up includes imaging to ensure filter position, periodic blood clot assessments, and scheduling timely filter removal once the risk subsides.
Your well-being is our top priority. Reach out today to discover how our dedicated team can support your health journey.
Have questions or want to learn more? Use the form below to get started!
Connect with South Florida’s trusted multispecialty care team and take control of your health with compassion and convenience.
©2025 South Florida Multispecialty Medical Group. All Rights Reserved.