Staying ahead of a life-threatening condition like an aortic aneurysm begins with knowledge and we’re here to walk you through exactly what you need to know. Aortic aneurysms often develop silently, but with proper screening, timely diagnosis, and expert care, outcomes can improve significantly. At South Florida Multispecialty Hospital, our team of vascular experts combines leading technology with patient-centered care to help you navigate this complex condition with confidence.
An aortic aneurysm is a bulge or ballooning in a section of the aorta, the main artery responsible for transporting blood from the heart to the rest of the body. Think of a weak spot on a garden hose; under pressure, it swells and can eventually burst. That’s what we worry about most: the risk of a rupture. Left undetected, a rupture can lead to life-threatening internal bleeding within minutes.
Simply put, aneurysms represent a structural weakness in one of our most vital blood vessels. They’re dangerous, often silent, and more common than many realize.
The two major types of aortic aneurysms depend on where they occur:
These develop in the section of the aorta that passes through the abdomen. They’re more prevalent than thoracic aneurysms and often diagnosed during routine imaging or screening for unrelated issues.
These occur in the chest cavity and may involve the ascending, arch, or descending parts of the thoracic aorta. They tend to be more closely associated with genetic disorders like Marfan syndrome or trauma from high-speed injury.
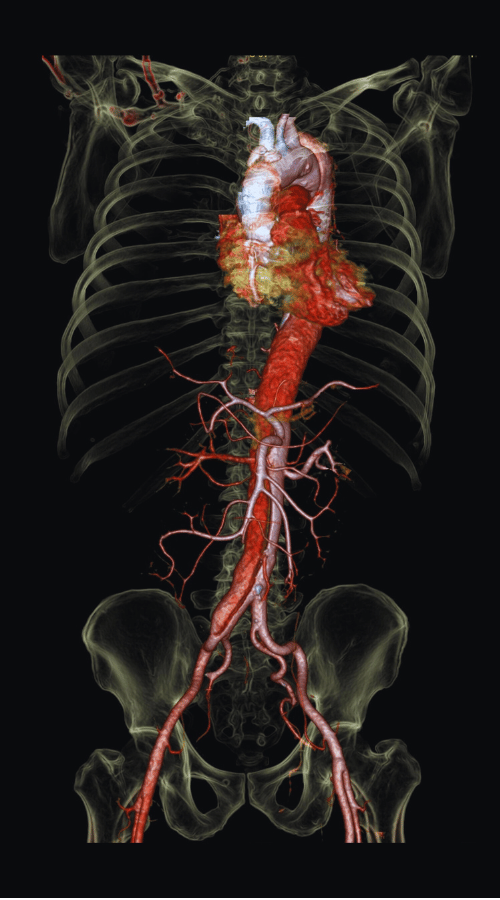
At its core, an aneurysm forms when plaque buildup, blood pressure, aging, or genetic factors weaken the wall of the aorta over time. As the layers of the vessel lose integrity, the internal pressure causes it to balloon outward.
Aneurysms grow silently and gradually. Often, we don’t discover them until they pose a real threat. That’s why awareness and early screening matter so much. Chronic inflammation, enzymes that degrade tissue, and connective tissue disorders often exacerbate the risk.
The tricky part? Many people with aortic aneurysms experience no symptoms at all until the aneurysm has grown substantially or ruptured. However, when symptoms do appear, they might include:
We’ve seen patients come in with vague abdominal discomfort, thinking it’s indigestion, only to find a large aneurysm requiring immediate intervention. Understanding these subtle signs can tip the balance between crisis and control.
Certain people are more vulnerable to developing aortic aneurysms than others. Common risk factors include:
If you or a loved one fall into any of these categories, talk to a healthcare professional about screening.
Early detection can literally be life-saving. Here’s how we usually identify aortic aneurysms:
A fast, non-invasive scan to detect size and shape, perfect for routine screening in older men with a history of smoking.
Provides a detailed view of the aorta with contrast dye, allowing us to measure the aneurysm and plan interventions.
Another high-resolution option that’s especially helpful in patients with allergies to certain contrast agents or radiation concerns.
The U.S. Preventive Services Task Force recommends one-time screening for AAA in men aged 65 to 75 who have smoked. If you fit that profile or have a family history, don’t wait.
Once diagnosed, we decide between two main treatment tracks:
If an aneurysm is small (less than 5.5 cm for AAA), we may choose to simply monitor its progress through regular imaging. In many cases, it can remain stable for years.
When aneurysms grow or symptoms appear, timely surgery becomes necessary. Two main approaches are available:
Our vascular surgeons at South Florida Multispecialty Hospital are skilled in both open and minimally invasive repair techniques, allowing us to tailor care to your specific needs.
Post-procedure care involves careful wound healing, medications to control blood pressure, and regular imaging to monitor the repair. After EVAR, follow-up scans are crucial to check for endoleaks, when blood leaks into the aneurysm sac outside the graft.
Patients who undergo either type of repair enter a lifelong monitoring program. We also provide guidance on medications, physical activity, nutrition, and smoking cessation to prevent recurrence or complications.
Can aortic aneurysms be prevented? Not entirely, but we can significantly reduce risk. Here’s how:
We’ve had patients avoid surgery entirely just from slowing aneurysm growth through these lifestyle modifications. Healthcare isn’t just about intervention, it’s about prevention, too.
If you or someone you know has risk factors or symptoms related to aortic aneurysms, don’t wait. Schedule a vascular consultation with our experts at South Florida Multispecialty Hospital because early detection can change everything.
An aortic aneurysm is a bulge in the aorta caused by a weakened vessel wall. Over time, as pressure builds, the aorta can expand and potentially rupture—especially if no treatment is initiated.
Most are asymptomatic. However, symptoms when present include pain in the chest, back, or abdomen, a pulsating abdominal mass, hoarseness, or trouble breathing.
Smokers, older adults (especially males over 65), those with high blood pressure or a family history, and individuals with connective tissue disorders are at heightened risk.
Ultrasounds, CT scans, or MRIs are the most common imaging tools. Screening is particularly vital for men aged 65–75 who have smoked.
Treatment ranges from surveillance for smaller aneurysms to surgery either open repair or a less invasive procedure called EVAR.
Location. AAAs occur in the abdomen; TAAs in the chest. Symptoms and management strategies vary depending on their location.
Quitting smoking, controlling blood pressure and cholesterol, and healthy lifestyle habits can slow aneurysm growth or prevent further complications.
Initial hospitalization, followed by weeks of recovery, and long-term imaging to assess the surgical site. EVAR patients tend to recover faster.
Yes. Genetic syndromes like Marfan and Ehlers-Danlos, as well as family history, increase the likelihood of aneurysm formation.
Monitoring frequency varies by aneurysm size but typically involves imaging every 6–12 months under guidance from your vascular team.
Your well-being is our top priority. Reach out today to discover how our dedicated team can support your health journey.
Have questions or want to learn more? Use the form below to get started!
Connect with South Florida’s trusted multispecialty care team and take control of your health with compassion and convenience.
©2025 South Florida Multispecialty Medical Group. All Rights Reserved.