Let’s face it, heart disease isn’t just another health concern. It’s the world’s number one cause of death, claiming millions of lives every year. But here’s the good news: we’ve come a long way in managing it, especially when it comes to diagnosing and treating blocked arteries. At the heart of this progress are three powerful tools: angiogram, angioplasty, and stenting.
These aren’t just medical terms. They’re life-saving procedures that help us understand the problem, open up narrowed arteries, and keep them open. And for someone experiencing chest pain or shortness of breath, these interventions could be the difference between a life-threatening heart attack and a fast recovery.
An angiogram is our window into your heart’s arteries. We perform this minimally invasive test by inserting a thin catheter, usually through the wrist or groin, and guiding it up to the arteries of the heart. Then, we inject a contrast dye that lights up the blood vessels on X-ray images.
What we’re looking for is simple but critical: blockages, narrowing, or abnormal structures. It helps us determine whether further intervention, like angioplasty or stenting, is needed.
In short, angiograms play an essential diagnostic role. We can’t fix what we can’t see.
Once we’ve found a significant blockage, the next step is angioplasty. Here’s how it works: a balloon-tipped catheter is fed to the blocked site. When inflated, it compresses the plaque against the artery wall, widening the path for blood flow.
This process is incredibly efficient and often performed during the same session as the diagnostic angiogram. The best part? It’s usually done under local anesthesia and allows for a fast recovery.
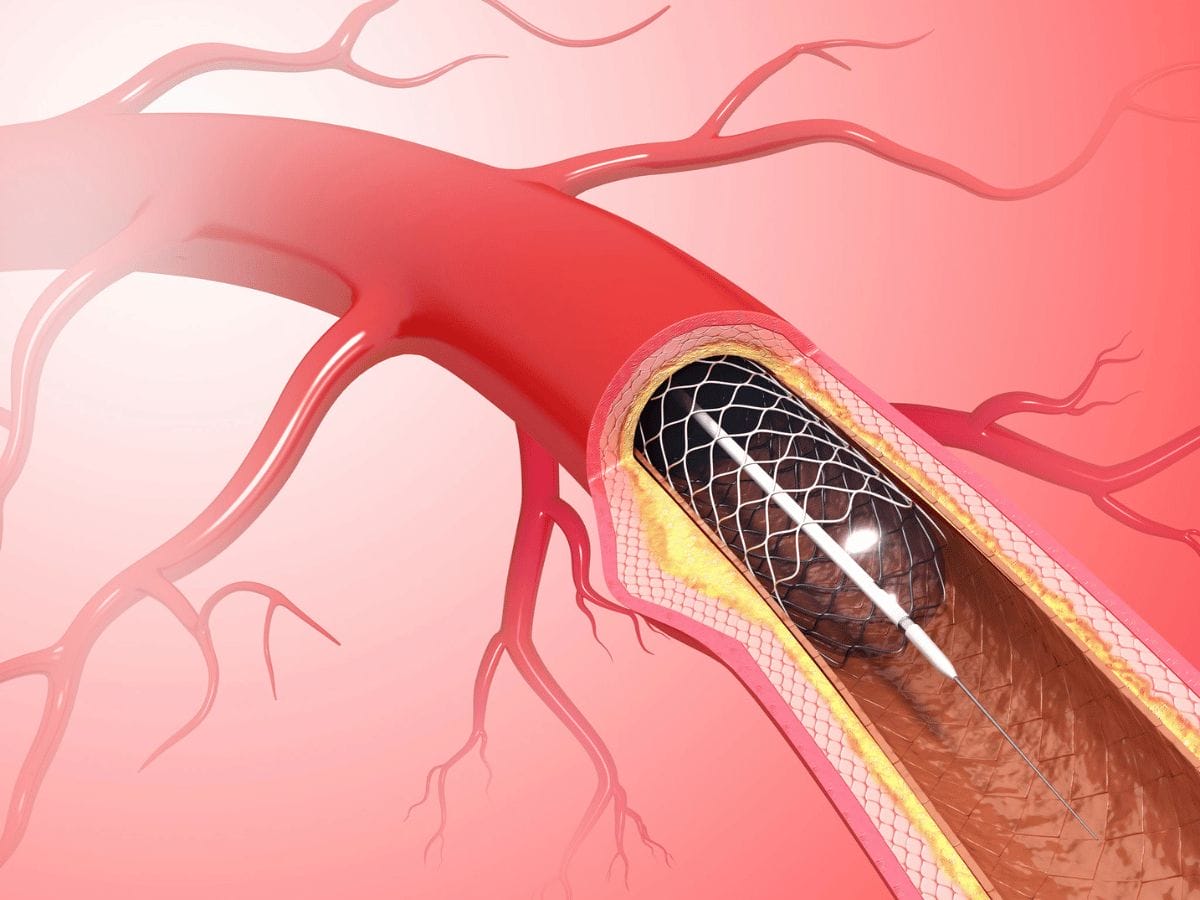
In most cases, angioplasty isn’t enough on its own. After we deflate the balloon, there’s a risk the artery might narrow again. That’s where stents come in.
A stent is a tiny mesh tube that we place in the artery to keep it open. These days, the majority of stents are drug-eluting. That means they release medication to prevent scar tissue and reduce the risk of the artery closing again—a condition called restenosis.
Stents bridge the gap between temporary relief and long-term success.
Not every patient experiencing chest pain needs these procedures. Here’s when they typically come into play:
Heart teams weigh factors like symptoms, medical history, and test results before recommending these treatments.
Let’s walk through what to expect, step by step.
Minimally invasive, highly effective, and often quick to recover from angioplasty and stenting have transformed cardiac care. But they’re not without risks, which include:
Fortunately, complications are rare when these procedures are performed by experienced providers under the right conditions.
We’re continually evolving these techniques. Some of the latest innovations include:
We align our approach with the latest medical research and guidelines from trusted bodies like the American Heart Association.
Your journey doesn’t end once the artery is opened, it’s just the beginning, and we’re here for every step.
We typically prescribe blood thinners, cholesterol-lowering drugs, and recommend lifestyle changes. These include:
Follow-up visits may include blood tests, EKGs, or stress tests to ensure you’re on the right path.
Understanding how angiogram, angioplasty, and stenting work empowers patients to take control of their heart health. These aren’t just procedures, they’re bridges to a longer, more active life. And when done at centers with skilled teams like South Florida Multispecialty Hospital, outcomes are even more optimistic.
If you or a loved one is experiencing chest discomfort, fatigue, or unexplained shortness of breath, don’t wait. Early action can change everything.
Think you might need an angiogram or heart exam? Our cardiology team at South Florida Multispecialty Hospital is ready to help. Reach out today and let’s take a closer look together, we can keep your heart strong and your future brighter.
An angiogram is an X-ray imaging test that uses a contrast dye and catheter to visualize blockages or abnormalities in arteries. It's often the first step in diagnosing coronary artery disease.
Angioplasty is typically recommended when a significant blockage is found during an angiogram, especially in patients with symptoms like chest pain or evidence of reduced blood flow.
A stent acts as a scaffold inside the artery. Once placed during angioplasty, it prevents the artery from collapsing or narrowing again. Drug-eluting stents release medication to prevent scar tissue.
Although generally safe, risks include bleeding, contrast dye reaction, restenosis, or very rarely, heart attack or stroke. Most risks are minimal when managed appropriately.
Patients are usually asked to fast, temporarily stop certain medications, and arrive a few hours early for pre-op evaluation. Your care team will guide you through specifics.
Most patients recover within a few days, with some resuming light activities in 24-48 hours. Full recovery may take about a week.
Yes. Most patients need to remain on medications, adopt healthier diets, and exercise regularly. Lifelong changes improve outcomes significantly.
Modern stents, especially drug-eluting types, reduce restenosis rates and improve long-term artery patency. They're becoming more biocompatible and safer.
You may stay for several hours or overnight. Monitoring includes heart rhythm, bleeding at catheter site, and ensuring the procedure was successful.
Yes. If a stented artery narrows again, a repeat angioplasty or bypass surgery may be considered based on the situation.
Your well-being is our top priority. Reach out today to discover how our dedicated team can support your health journey.
Have questions or want to learn more? Use the form below to get started!
Connect with South Florida’s trusted multispecialty care team and take control of your health with compassion and convenience.
©2025 South Florida Multispecialty Medical Group. All Rights Reserved.