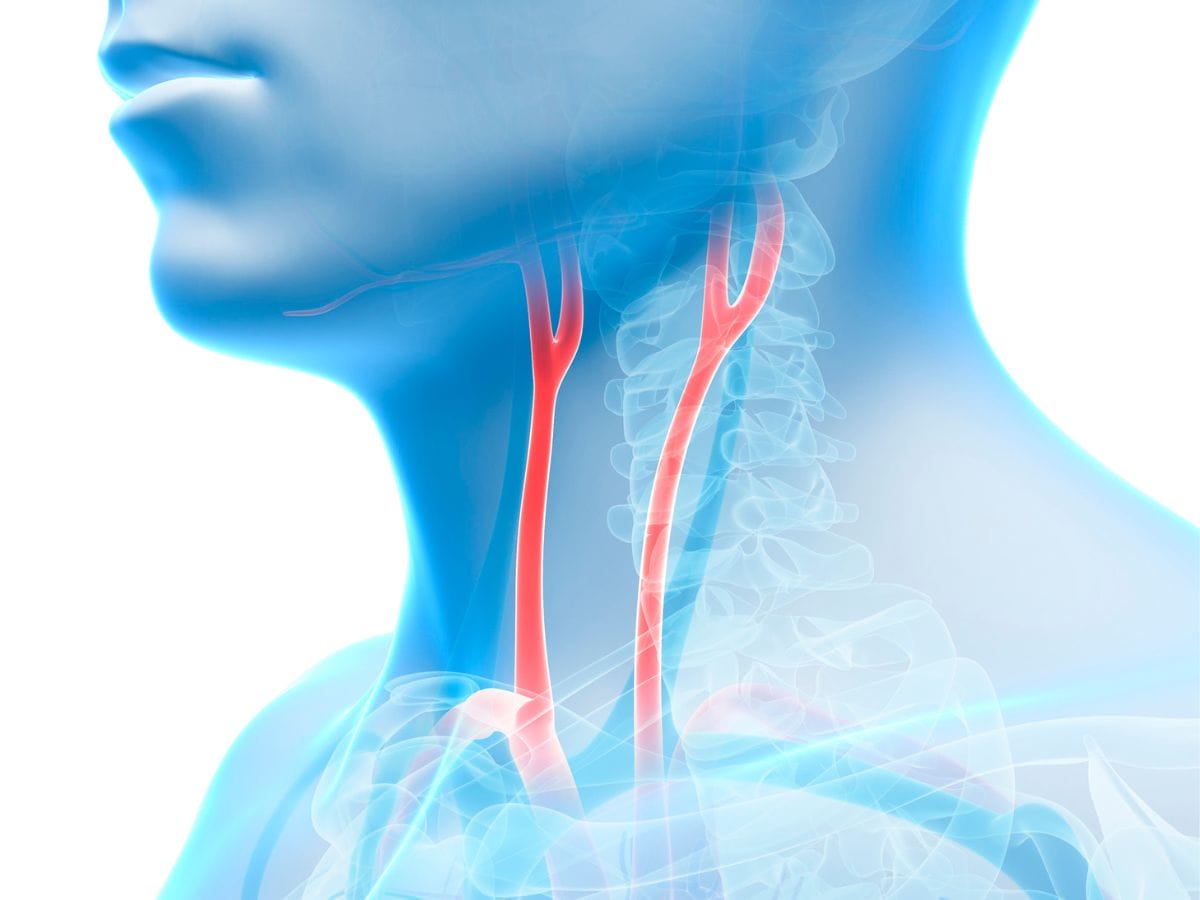
Carotid artery disease occurs when fatty deposits, often cholesterol and other substances, accumulate inside the carotid arteries that supply blood to the brain. This narrowing blocks blood flow, increasing the chance of a stroke.
Common symptoms include:
While some people don’t show symptoms, an ultrasound or evaluation due to other vascular issues might reveal the presence of significant stenosis.
Carotid endarterectomy has been the gold-standard surgical procedure for decades. Here’s how it works:
During this operation, a vascular surgeon makes an incision along the side of the neck, opens the blocked carotid artery, and physically removes the plaque. Once cleaned out, the artery is stitched back together, typically with a patch to widen the vessel safely.
We usually recommend carotid endarterectomy for symptomatic patients and certain high-risk asymptomatic individuals, depending on their stroke risk profile.
For patients who may not tolerate surgery well, due to age, prior neck surgery, or challenging anatomy, carotid artery stenting has proven to be a strong alternative.
Here’s how CAS works:
A thin catheter is inserted into a blood vessel, often through the groin, and guided to the carotid artery. A small balloon may be used to open the narrowed area. Then, a mesh-like, cylindrical stent is placed to keep the artery open. The procedure requires no large incisions and typically offers a quicker recovery.
Both treatments aim to achieve one goal: restore and maintain healthy blood flow to the brain to reduce the risk of ischemic stroke.
The key distinction lies in approach, invasiveness, anesthesia requirements, and in some cases, outcomes.
We base the treatment decision on clinical evidence, anatomical structure, and the individual’s overall health.
CEA is ideal for:
CAS might be preferable for:
This isn’t one-size-fits-all. Collaboration between the vascular surgery team, neurologists, and radiologists is essential in choosing the best route forward.
While both procedures are effective, each comes with its own set of advantages and risks.
Several high-profile studies, including those published by the Journal of Vascular Surgery and American Heart Association, show comparable long-term outcomes between the two procedures when applied to the right patients.
In younger individuals without comorbidities, CEA might offer slightly better stroke prevention in the short term. In older patients or those with complex neck anatomy, stenting offers a safer and more practical solution.
A tailored approach, taking all of this into consideration, is the cornerstone of modern stroke prevention.
Imaging doesn’t just help diagnose carotid artery disease, it helps guide treatment, too.
These diagnostics let us choose not only the best treatment but also the right timing.
Recovery times vary based on the procedure:
Long-term care involves:
Having a procedure doesn’t mean the end of vigilance, it’s often just the beginning of a healthier lifestyle.
We work with patients to address:
Partnering with a care team helps ensure success not just in the short term, but over a lifetime.
Get Expert Help from SFL Medical Group Now
If you or a loved one is experiencing symptoms of carotid artery disease, or have been told you may need surgery, don’t wait. Our team at South Florida Multispecialty Medical Group can evaluate your case, guide you through next steps, and help you make an informed decision tailored to your health and goals. Schedule a consultation now.
Carotid endarterectomy is an open surgical procedure where the surgeon removes fatty plaque from the inner walls of the carotid artery to restore proper brain blood flow and lower stroke risk.
Stenting uses a catheter to place a mesh stent within the narrowed artery. It’s less invasive than endarterectomy and better suited for people who can’t undergo surgery safely.
CEA is often preferred for younger, healthier patients with severe narrowing. CAS may be better for older adults or those with other health conditions or prior neck surgeries.
CEA may include risks like infection and nerve injury, while CAS may involve an increased risk of embolic stroke or artery re-narrowing in specific patients.
We assess several factors: degree of narrowing, symptom presence, overall health, anatomy, and surgical risk—then recommend the safest, most effective route.
CEA takes about 2–3 weeks for full recovery. CAS patients usually return to normal activities within a few days and often go home the day after the procedure.
Both are highly effective. With the right patient selection, each dramatically reduces the risk of stroke and improves long-term outcomes.
Yes. Ongoing risk factor management, medication adherence, follow-up imaging, and lifestyle improvements are essential to maintain vessel health long term.
Most major insurance providers including Medicare cover both procedures if indicated. Coverage often depends on meeting specific clinical criteria and imaging findings.
Regular follow-up includes ultrasound imaging to monitor artery status, as well as routine cardiovascular checkups with your care team.
Your well-being is our top priority. Reach out today to discover how our dedicated team can support your health journey.
Have questions or want to learn more? Use the form below to get started!
Connect with South Florida’s trusted multispecialty care team and take control of your health with compassion and convenience.
©2025 South Florida Multispecialty Medical Group. All Rights Reserved.