Gout is not just “a rich man’s disease,” as we’ve often heard. It’s a complex and painful form of inflammatory arthritis that affects over 8 million people in the United States alone. This condition occurs when high levels of uric acid in the blood, known as hyperuricemia, lead to the formation of sharp monosodium urate crystals in the joints. These crystals cause sudden, intense pain, swelling, and tenderness, typically in the big toe but not exclusively.
For many of us, gout doesn’t just impact physical mobility, it disrupts quality of life, interrupting sleep, affecting work, and even causing anxiety about the next flare-up. But with proper care and understanding, gout is incredibly manageable.
Let’s get into the “why” behind this disease. Gout occurs due to increased production or decreased excretion of uric acid. Uric acid is a normal byproduct of purine metabolism—purines being natural substances found both in our body and in certain foods.
Several risk factors increase the likelihood of experiencing gout:
Men are more likely to develop gout than women, at least until menopause, after which the risk increases for women as well.
South Florida’s diverse and vibrant lifestyle—often rich in seafood, wine, and backyard barbecues—could unknowingly lead to higher exposure to dietary triggers of gout.
Understanding what’s happening beneath the surface can empower us to take control. Gout begins with uric acid accumulation, often due to either the body making too much or not eliminating enough through the kidneys. When uric acid accumulates beyond a certain point, it forms needle-like crystals in joint spaces.
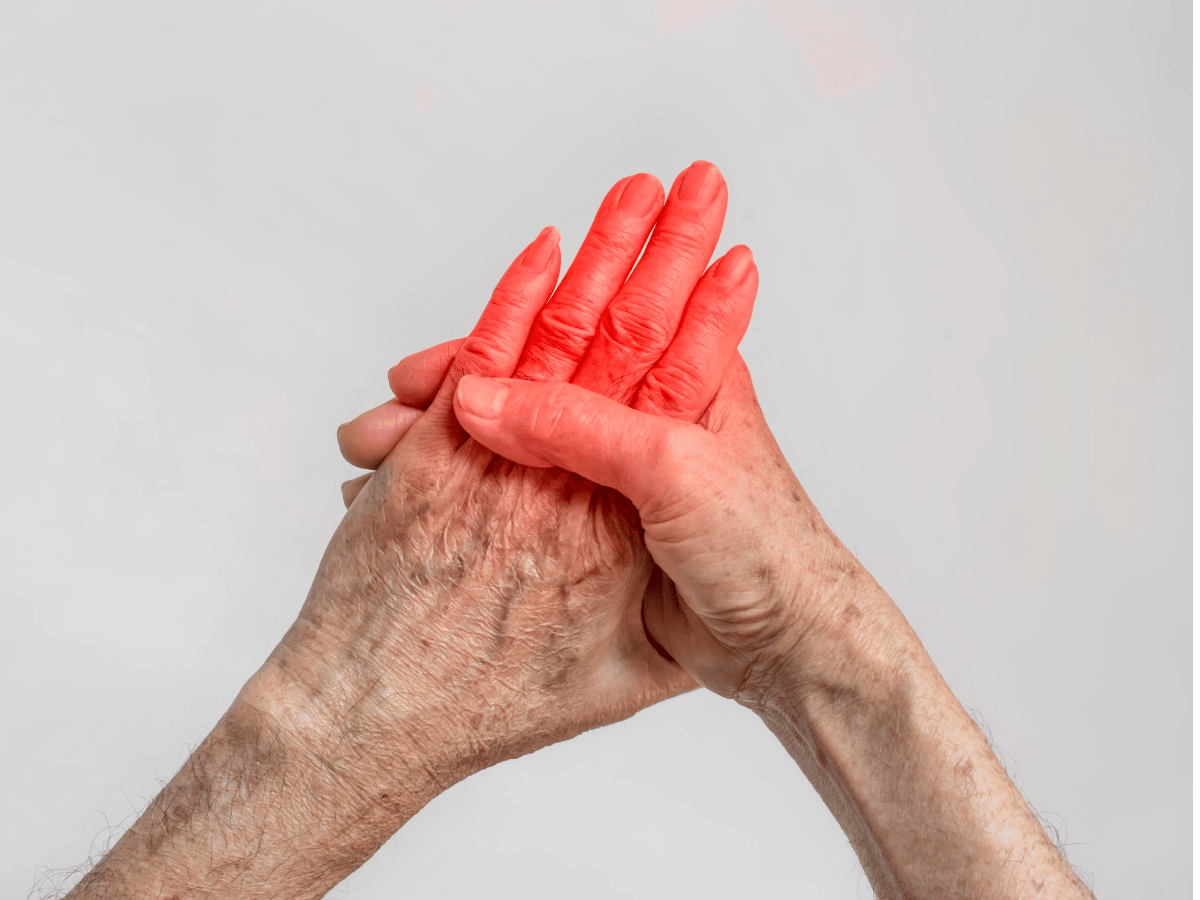
The immune system identifies these crystals as intruders, launching an inflammatory response. That’s when pain, redness, warmth, and swelling kick in—commonly affecting one joint at a time.
In chronic cases, untreated gout can lead to tophi—visible, lumpy collections of urate crystals under the skin—and permanent joint damage.
Most people describe a gout attack as waking up in the middle of the night with searing joint pain, especially in the big toe. But it can affect other joints too, including knees, ankles, elbows, fingers, and wrists.
Key symptoms include:
If you’ve experienced these signs, especially if they recur, it’s time to consult a specialist.
A proper diagnosis sets the tone for successful treatment. Physicians typically start with a clinical examination and a detailed health history. They might ask about your diet, alcohol intake, medication use, and family history.
To confirm gout, your doctor might perform:
Managing the pain of a flare-up is the immediate priority. Fortunately, multiple treatment options are available:
Prompt treatment can reduce attack duration and get you back on your feet sooner.
Treating gout isn’t just about handling flare-ups, it’s about preventing them. That’s where urate-lowering therapy comes into play.
Common long-term medications include:
Doctors aim to keep blood uric acid levels below 6 mg/dL to minimize the risk of attacks and tophi formation. Regular monitoring ensures therapy is effective and appropriately adjusted.
Managing gout goes beyond pills. Lifestyle plays a huge role in slowing or preventing progression.
Here’s what helps:
A registered dietitian or nutritionist can be a powerful ally in crafting a gout-friendly meal plan.
Living well with gout involves awareness and preparation. Here’s what we recommend:
When supported by a team—including primary care providers, rheumatologists, and sometimes dietitians—patients living with gout can thrive.
Don’t try to tough it out. If you experience any of the following, reach out to your healthcare provider promptly:
Prompt intervention can make a lasting difference in managing gout and protecting joint function.
If you’re experiencing severe joint pain, swelling, or repeated gout flare-ups, don’t wait. Connect with the expert team at South Florida Multispecialty Hospital today. Personalized care, knowledgeable specialists, and long-term solutions are just a call or click away.
Gout is a type of arthritis triggered by high levels of uric acid in the bloodstream. When uric acid crystallizes in the joints, it causes intense inflammation and pain, especially in the big toe and other extremities.
Risk factors include a high-purine diet, alcohol consumption, obesity, certain medications, kidney problems, and a family history of gout. Men and post-menopausal women are particularly prone.
Symptoms often include sudden, severe joint pain, redness, swelling, warmth, and restricted movement—most commonly occurring at night in one joint.
Diagnosis involves physical examination, joint fluid analysis (to detect urate crystals), blood tests, imaging studies (like ultrasound or X-rays), and patient history.
Doctors may prescribe NSAIDs, colchicine, or corticosteroids. Rapid treatment reduces pain and prevents prolonged discomfort.
Limiting high-purine foods, alcohol, and sugary drinks while emphasizing plant-based foods and hydration can help manage uric acid levels and reduce flare-ups.
Yes. Chronic gout can lead to joint damage, kidney stones, and tophi—crystal deposits under the skin. Long-term control is important for preserving mobility and health.
Adopting a healthy diet, losing excess weight, exercising regularly, staying hydrated, and avoiding known dietary triggers are key strategies that reduce gout recurrence.
Your well-being is our top priority. Reach out today to discover how our dedicated team can support your health journey.
Have questions or want to learn more? Use the form below to get started!
Connect with South Florida’s trusted multispecialty care team and take control of your health with compassion and convenience.
©2025 South Florida Multispecialty Medical Group. All Rights Reserved.