
MIS Bunion Surgery vs Traditional: Which Is Right for You?
If you’re dealing with daily discomfort, swelling, or misshapen toes from a bunion, you’re not alone. Bunion deformities don’t discriminate, they affect people of

When we think of diabetes symptoms, our thoughts often turn to thirst, fatigue, or fluctuating blood sugar levels. But few in Miami or anywhere realize that toenails can offer some of the earliest, most visible signs of diabetes, especially in its first stage. At SFL Medical Group, we’ve seen countless patients whose diagnoses began with their feet.
Diabetes impacts circulation and nerve health and there are few places in the body more sensitive to both than your feet. When blood flow decreases and nerves become damaged (a condition called peripheral neuropathy), small issues can become big problems.
Fingernails usually get more attention in self-care routines, but toenails tell a quieter, often more medically revealing story. Poor blood circulation to the lower limbs and impaired immune responses from elevated glucose levels can lead to nail changes such as thickening, discoloration, or delayed growth.
Most of the early warning signs in the nails are subtle, and many people brush them off. Here are the specific changes we look for in our patients:
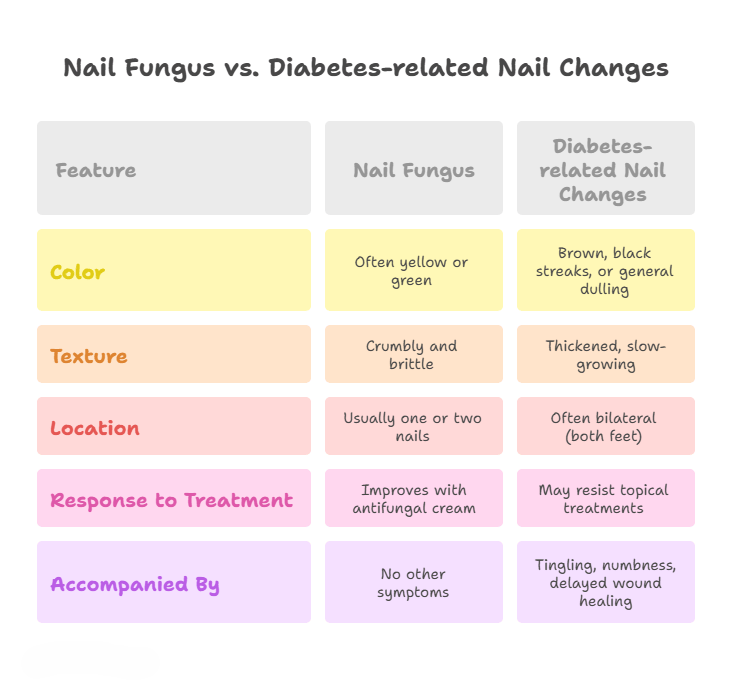
Watch for a yellowish or brown tint, even gray or black streaks under the nail. Dark lines, also called melanonychia, may indicate underlying trauma or even disease. While people in Miami’s sunny climate may attribute nail discoloration to footwear or activity, prolonged yellowing alongside brittle nails may point toward diabetic changes.
This can resemble fungal infections but is often a circulatory issue. Diabetics may have nails that grow slower but get thicker, making trimming difficult.
This condition is more common than patients expect. Many assume they’ve stubbed their toe, but onycholysis (separation of nail from the bed) can also be caused by reduced oxygen supply to tissues, very common in early diabetes.
Due to poor healing and immune response, diabetics are at greater risk of skin infections around the nail bed, particularly where there’s an ingrown nail or cuticle damage.
Nails that don’t seem to grow over months, even with adequate care may hint at disrupted metabolic function, including poor glucose control.
Diabetics often experience recurring infections or fungal issues that seem resistant to treatment. This includes onychomycosis, a tough nail fungus notorious for affecting diabetic feet.
A common question we get at our Miami clinics is this: “How do I know if it’s just fungus or something more serious like diabetes?”
When in doubt, consult a podiatrist.
Ignoring nail changes in early diabetes can lead to dangerous outcomes, including:
At SFL Medical Group, we’ve witnessed cases where a simple nail abnormality was the only early clue before more serious complications began. That’s why catching it early matters, especially in the subtropical heat of Miami, where foot issues can simmer unseen in closed shoes.
When you visit SFL Medical Group, we’ll begin with three essential steps:
Using magnification and light tools, we examine the nail plate, bed, surrounding skin, and symmetry of both feet.
To confirm a diabetes diagnosis, we test fasting blood glucose and A1C markers.
In persistent cases (e.g., suspected subungual melanoma or resistant infection), nail clippings may be analyzed, and in rare cases, biopsy requested.
Good foot care is non-negotiable especially here in Miami, where open-toed shoes might expose feet to environment related trauma. Here’s what we recommend:
Look for swelling, redness, or any nail change. If you can’t see the bottom of your feet, use a mirror or have a family member help.
Wash your feet with gentle soap, dry thoroughly (especially between toes), and moisturize around but not under the nail bed.
Cut across the nail rather than rounding the corners. Avoid overly short trimming, which raises the risk of ingrown nails.
Breathable, padded, fitted shoes prevent both trauma and excessive moisture, which can promote fungi.
People with prediabetes or Type 2 diabetes should see a podiatrist every 6 to 12 months, even without active concerns.
If you notice:
Contact our team at SFL Medical Group. Infections in diabetic patients escalate quickly and must be addressed fast.
More To Explore

If you’re dealing with daily discomfort, swelling, or misshapen toes from a bunion, you’re not alone. Bunion deformities don’t discriminate, they affect people of

Why Vascular Imaging Matters More Than Most People Realize Blocked or weakened blood vessels often stay silent until something serious happens. Many patients in South

©2025 South Florida Multispecialty Medical Group. All Rights Reserved.