
Tailor’s Bunion: Causes, Symptoms & Treatment in Miami
Understanding Tailor’s Bunion (Bunionette): More Than Just a “Small Bunion” Many people recognize bunions at the big toe. Fewer realize a similar problem can
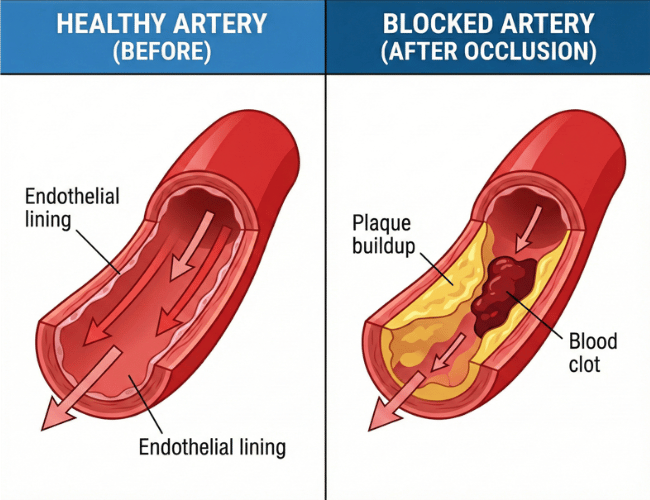
When an artery suddenly becomes blocked, cutting off blood supply to an organ or limb, the resulting condition is known as acute arterial occlusion. This is an emergency, prompt action is critical to prevent permanent damage, and in many cases, to save a life.
At SFL Medical Group, we’ve seen how fast and devastating this condition can be. In one instance, a patient arrived within an hour of sudden leg pain and numbness. Thanks to our vascular team’s immediate intervention, we successfully salvaged the limb and avoided long-term complications. But not every patient is as fortunate. Delayed treatment can lead to irreversible tissue death or even death.
Acute arterial occlusion happens when blood flow through an artery is abruptly obstructed. This can stop oxygen and nutrients from reaching downstream tissues.
The most common causes include:
The most common sites of acute arterial occlusion include the lower extremities, particularly the femoral and popliteal arteries. However, it can also affect renal arteries, upper limbs, mesenteric arteries, or even arteries supplying the brain (which leads to strokes).
Acute arterial occlusion symptoms depend on where the blockage occurs. In all cases, symptoms usually arise suddenly. With our vascular specialists at SFL Medical Group, we emphasize early recognition because there’s often a short therapeutic window.
In limb occlusion cases, remember the “Six Ps” of ischemia:
In mesenteric (intestinal) occlusion, intense abdominal pain that’s disproportionate to exam findings is a red flag.
Renal arterial occlusion can cause flank pain, nausea, vomiting, and acute kidney injury.
Our interventional specialists are trained to recognize subtle nuances between ischemic conditions because every second counts.
At SFL Medical Group, our approach includes rapid imaging and lab work. When acute arterial occlusion is suspected, we don’t wait. Immediate diagnostics start with:
In some emergencies, a direct surgical exploration may be needed without delay, skipping non-essential diagnostics when time is critical.
Managing acute arterial occlusion is a race. The longer a tissue goes without oxygen, the more damage accumulates. At SFL Medical Group, we combine surgical expertise with endovascular precision to ensure the most effective treatment. Here’s what our patients can expect:
In many cases, we use specialized catheters or surgical tools to physically remove the clot blocking the artery. This is particularly effective in acute embolic events.
For some patients, minimally invasive techniques like catheter-based thrombolysis (injecting clot-dissolving medication directly into the site) are preferred. Stents or balloon angioplasty may also be used to restore vessel integrity.
If the artery cannot be salvaged or reopened, surgeons may create a bypass using either synthetic material or a healthy vein from the patient essentially rerouting blood flow around the occlusion.
Once flow is restored, we prevent further events with blood thinners and treat any underlying causes. Often, patients with atrial fibrillation or atherosclerosis will need long-term medication and follow-up care with our multispecialty teams.
Depending on how much damage was sustained before reperfusion, patients may require additional support especially if nerves or muscles were involved.
Our cardiovascular program works hand-in-hand with rehab specialists, physical therapy, and internal medicine to create an individualized follow-up plan. Some patients need wound-care services, others benefit more from gait training or occupational therapy.
We guide every step post-recovery to regain strength, minimize complications, and reduce risk of further vascular events.
While acute arterial occlusion can affect anyone, higher risk exists in:
Routine check-ups with our vascular medicine teams can help catch early warning signs. For some, we recommend diagnostic imaging to spot narrowed vessels before they cause obstruction.
If you or anyone you know experiences sudden numbness, pain, or a cold limb, that’s a medical emergency. Call 911 and keep the person warm and still.
Never try to “walk it off” or wait to see if it improves. Time isn’t on your side. The earlier we intervene, the greater the chance we save tissue and avoid amputation or organ failure.
If you or a loved one are at risk or have experienced symptoms, don’t wait. Reach out to us and schedule a consultation.
More To Explore

Understanding Tailor’s Bunion (Bunionette): More Than Just a “Small Bunion” Many people recognize bunions at the big toe. Fewer realize a similar problem can

Why Vascular Imaging Matters More Than Most People Realize Blocked or weakened blood vessels often stay silent until something serious happens. Many patients in South

©2025 South Florida Multispecialty Medical Group. All Rights Reserved.